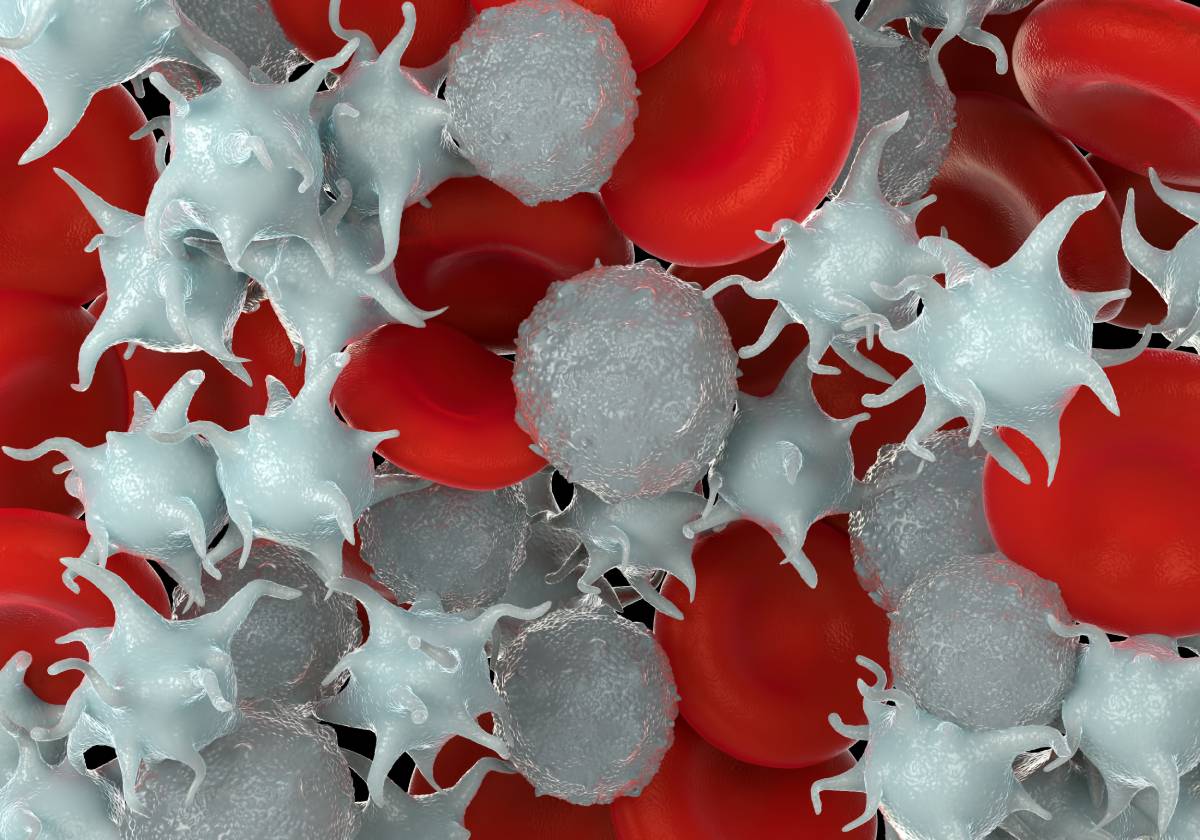
Platelets, created by megakaryocytes in our bone marrow, respond to bleeding by aiding in blood clot formation (Greenberg & Kaled, 2013). These components of our blood have a lifespan of 7 to 10 days. Thrombocytopenia, also known as a platelet count less than 150,000/uL, is due to various causes (Greenberg & Kaled, 2013). Mild thrombocytopenia occurs with a platelet count between 70,000/u/L and 150,000/uL, while severe thrombocytopenia is indicated by a count below 20,000/uL (Greenberg & Kaled, 2013). Although thrombocytopenia can manifest differently in different patients, most patients will be symptomatic if platelet count drops to less than 50,000/uL (Greenberg & Kaled, 2013). General causes of low platelets include decreased production, increased destruction, sequestration in the spleen, and dilution of blood (Smock & Perkins, 2014).
Primary neoplastic disorders of the bone marrow are commonly known causes of low platelets. Examples include acute myeloid leukemia, myelodysplastic syndrome, myeloproliferative syndrome, acute lymphoid leukemia, hairy cell leukemia, chronic lymphoid leukemia, non-Hodgkin lymphoma and multiple myeloma (Greenberg & Kaled, 2013). Treatments for various neoplastic disorders, including radiotherapy and chemotherapy can also lead to thrombocytopenia.
Idiopathic thrombocytopenia purpura (ITP) is a relatively common condition caused by decreased platelet production and autoantibodies against platelets. It can develop as a primary condition or be secondary to other autoimmune disorders, including systemic lupus erythematosus, Grave disease, and sarcoidosis (Smock & Perkins, 2014). This condition is treated with corticosteroids, intravenous immunoglobulin, anti-RhD and splenectomy if necessary (Smock & Perkins, 2014).
Medications associated with thrombocytopenia, including chemotherapeutic agents as previously mentioned, include linezolid, an antibiotic, and heparin, a blood thinner (Greenberg & Kaled, 2013). Other causes of drug-induced immune thrombocytopenia include sulfonamides, ampicillin, vancomycin, piperacillin, acetaminophen, and many others. These may lead to thrombocytopenia through an immune or non-immune mediated mechanism (Sruthi & Khandhar, 2023). Sometimes it is difficult to determine which agent is the cause of drug-induced thrombocytopenia. General treatment is to discontinue the offending agent and prevent further complications (Greenberg & Kaled, 2013).
Certain viral infections are also relevant causes of low platelets. Some examples include human immunodeficiency virus, hepatitis B, hepatitis C, Epstein-Barr virus, cytometalovirus, parvovirus B19, varicella-zoster, rubella, and mumps. These infections can cause bone marrow suppression (Greenberg & Kaled, 2013). Tuberculosis, a bacterial infection, and malaria, a parasitic infection can also affect platelet count (Greenberg & Kaled, 2013).
The hormone thrombopoietin, produced primarily in the liver, is a stimulator of platelet creation and maturation. Alcoholism, a common cause of cirrhosis, is a liver-related cause of thrombocytopenia (Greenberg & Kaled, 2013).
Other non-immune mediated causes of low platelets include thrombocytopenic purpura (TTP), hemolytic uremic syndrome (HUS), and disseminated intravascular coagulation (DIC). TTP occurs due to antibodies against the enzyme ADAMTS13, resulting in decreased breakdown of von Willebrand factor resulting in thrombocytopenia due to microvascular thrombi (Smock & Perkins, 2014). HUS often occurs after infectious diarrhea due to production of Shiga toxin by the bacteria leading to thrombotic microangiopathy. Atypical HUS may occur due to abnormalities of the alternative complement system and is heritable (Smock & Perkins, 2014). DIC occurs when blood clots form throughout the body, leading to consumption of clotting factors and platelets, and has a variety of causes not limited to but including sepsis, surgery, major trauma, and cancer (Smock & Perkins, 2014).
As a final note, thrombocytopenia can also occur in pregnancy. Gestational thrombocytopenia is an asymptomatic condition that occurs in pregnancy due to increased plasma volume (Greenberg & Kaled, 2013). Thrombocytopenia can occur in a more serious form in pregnancy including preeclampsia, eclampsia, and HELLP syndrome. These are life threatening diseases, one of the most serious being DIC, as previously mentioned (Greenberg & Kaled, 2013).
Ultimately thrombocytopenia is due to a variety of unique and diverse causes. After stabilizing symptomatic patients, providers must carefully assess and determine the cause prior to pursuing treatment, starting with if platelet production is suppressed, or if there is increased platelet destruction or sequestration or a combination of these. Then, they may proceed with treatment.
References
Greenberg, Edythe M, and Elizabeth S Kaled. “Thrombocytopenia.” Critical care nursing clinics of North America vol. 25,4 (2013): 427-34, v. doi:10.1016/j.ccell.2013.08.003
Smock, K J, and S L Perkins. “Thrombocytopenia: an update.” International journal of laboratory hematology vol. 36,3 (2014): 269-78. doi:10.1111/ijlh.12214
Sruthi, Jinna, and Paras B. Khandhar. “Thrombocytopenia – StatPearls – NCBI Bookshelf.” National Library of Medicine, StatPearls, 4 July 2023, www.ncbi.nlm.nih.gov/books/NBK542208/.